Overdose and Poisonings
Anticholinergic/Organophosphates
Antipsychotics/Acute Dystonic Reaction
Beta Blocker Toxicity
Calcium Channel Blockers
Carbon Monoxide
Clonidine
Cocaine and Sympathomimetic Overdose
Cyanide Toxicity and Smoke Inhalation
HAZMAT Alert
Tricyclic and Tetracyclic Antidepressant Overdose
General
Determine the agent(s) involved, the time of the ingestion/exposure, and the amount ingested. Bring empty pill bottles, etc., to the receiving facility. Give nothing by mouth unless specified in protocol or directed by the Regional Poison Control Center. In the event that the poison control center gives recommendations that are not contained within these protocols, EMS providers should contact Medical Control for authorization to carry out the instructions.
Anticholinergic/Organophosphate Poisoning
Organophosphates cause acetylcholinesterase inhibition, resulting in signs and symptoms such as pinpoint pupils, eye pain, sweating, drooling, tearing, vomiting, seizures, and respiratory distress. Examples of commonly used organophosphate pesticides:
- Acephate (Orthene®)
- Azinphos-methyl (Azinphos®, Guthion®)
- Chlorpyrifos (Govern®, Lorsban®, Nufos®, Warhawk®, Whirlwind®)
- Diazinon
- Dimethoate (Cygon®)
- Disulfoton (Di-syston®)
- Ethoprop (Mocap®)
- Fenamiphos (Nemacur®)
- Malathion (Fyfanon®)
- Methamidophos (Monitor®)
- Methidathion (Supracide®)
- Methyl Parathion (Penncap-M®)
- Naled (Dibrom®)
- Oxydemeton-methyl (MSR®)
- Phorate (Thimet®)
- Phosmet (Imidan®)
- Profenofos (Curacron®)
Nerve agent chemical weapons such as Sarin, Soman, Tabun, and VX are also organophosphates and should be treated accordingly.
Basic Life Support
- Initiate HAZMAT Alert if indicated
- Wear protective clothing including masks, gloves, and eye protection
- Toxicity to ambulance crew may result from inhalation or topical exposure
- Remove all clothing and contain run-off of toxic chemicals when flushing
- Supplemental 100% oxygen
- Including ETCO2 level (35-45 normal)
Advanced Life Support
- Full ALS Assessment and Treatment
- If signs of severe toxicity, (severe respiratory distress, bradycardia, heavy respiratory secretions) – (do not rely on pupil constriction to diagnose or to titrate medications):
- Atropine 2 mg IV every 5 min; titrate dosing by assessing improvement in respiratory/ bronchial secretions
- For hypotension (systolic BP < 90 mmHg) not improved by fluid boluses, or when fluid\ boluses are contraindicated:
- Norepinephrine infusion at 0.5-16 mcg/minute IV/IO, titrated to maintain SBP > 90 mm Hg (see pg. 10-27 for infusion preparation chart) OR
- Push dose epinephrine: Remove 9ml (0.9mg) of 1:10,000 Epinephrine from the pre-filled syringe then draw 9ml of NS into the pre-filled syringe and mix solution. Concentration 10mcg/ml. IV push 1ml every minute to increase blood pressure to 90 mmHg; max 10ml (100mcg).
- If any of the following conditions occur, refer to the appropriate protocols:
- Altered Mental Status
- Seizures
Antipsychotics / Acute Dystonic Reaction
Example of commonly used medications that may result in acute dystonic reactions:
- Haloperidol
- Prolixin
- Thorazine
- Prochlorperazine (Compazine)
- Promethazine (Phenergan)
- Ziprasidone (Geodon)
Advanced Life Support
- Full ALS Assessment and Treatment
- For Dystonic reactions administer Diphenhydramine (Benadryl) 1 mg/kg IV (Max. 50 mg)
- May be administered IM if no IV access available
Beta Blocker Toxicity
Examples of commonly used Beta-Blocker medications:
- Single Agent Medication
- Propranolol (Inderal)
- Atenolol (Tenormin)
- Metoprolol (Lopressor)
- Nadolol (Corgard)
- Timolol (Blocadren)
- Labetolol (Trandate)
- Esmolol (Brevibloc)
- Carvedilol (Coreg)
- Combination Medication
- Corzide (nadolol/bendroflumethlazide)
- Inderide (Propranolol/HCTZ)
- Inderide LA (Propranolol/HCTZ)
- Lopressor HCT (Metoprolol/HCTZ)
- Tenoretic (Atenolol/Chlorthalidone)
- Timolide (Timolol/HCTZ)
- Ziac (Bisoprolol/HCTZ)
Advanced Life Support
- Full ALS Assessment and Treatment
- For patients with cardiovascular toxicity, defined by:
- SBP < 90 mm Hg
- Altered mental status
- Bradycardia
- 2nd or 3rd degree heart blocks
- Administer the following agents:
- NS 250 ml boluses IV (if hypotensive)
- Atropine 0.5 mg IV if Bradycardic
- Repeat every 3 minutes as needed (Maximum 3 mg)
- Glucagon 1mg IV/IO/IM/IN (pretreat with Zofran-see protocol)
- Calcium Chloride 1 gm IV/IO (pretreat with Zofran-see protocol)
- Contraindicated if patient is taking Digoxin or Lanoxin
- If no response, begin Transcutaneous Pacing
- If no response, start Epinephrine infusion at 2-10 mcg/minute IV/IO, titrated to BP and HR with improved clinical status of patient. (see infusion preparation chart)
Calcium Channel Blockers
Examples of commonly used Calcium Channel Blocker medication:
- Amlodipine (Norvasc)
- Nifedipine (Procardia, Adalat)
- Felodipine (Plendil, Renedil)
- Verapamil (Calan)
- Isradipine (DynaCirc)
- Diltiazem (Cardizem)
- Nicardipine (Cardene)
Advanced Life Support
- Full ALS Assessment and Treatment
- For patients with cardiovascular toxicity, defined by:
- SBP < 90 mm Hg
- Altered mental status
- Bradycardia
- 2nd or 3rd degree heart blocks
- Administer the following agents:
- NS 250 ml boluses IV (if hypotensive)
- Atropine 0.5 mg IV if bradycardic
- Repeat every 3 minutes as needed (Maximum 3 mg)
- If no response, Calcium Chloride 1 gram IV
- Contraindicated if patient taking digoxin (Lanoxin)
- If no response, may repeat Calcium Chloride 1 gram IV
- Glucagon 1mg IV/IO/IM/IN (pretreat with Zofran-see protocol)
- If no response, begin transcutaneous pacing
- If no response and hypotensive, administer push dose epinephrine: Remove 9ml (0.9mg) of 1:10,000 Epinephrine from the pre-filled syringe then draw 9ml of NS into the pre-filled syringe and mix solution. Concentration 10mcg/ml. IV push 1ml every minute to increase blood pressure to 90 mmHg; max 10ml (100mcg).
Carbon Monoxide
Signs and Symptoms:
Patients experiencing carbon monoxide inhalation exposure may experience any of the following signs and symptoms
- Headache
- weakness
- cutaneous flush
- coma
- anesthesia
- Dizziness
- nausea and or vomiting
- Tinnitus (ear ringing)
- paresthesias
Basic Life Support
- Remove the patient from the contamination source
- Personnel removing the patient(s) must wear the appropriate PPE
- Supplemental 100% oxygen; document time oxygen started
- Including ETCO2 level (35-45 normal)
- Keep patient as calm as possible to reduce metabolic oxygen needs
- Obtain baseline vital signs
- SPO2 may yield inaccurate reading based on the total content of carboxyhemoglobin
- For symptomatic patients, repeat vital signs every 10 minutes
- Monitor and record CO monitoring every 10 minutes
Advanced Life Support
- Full ALS Assessment and Treatment
- For smoke inhalation patients also consider Cyanide poisoning
- Support ventilator and respiratory efforts as necessary
- If impaired or compromised respiratory effort, ventilate with BVM and 100% O2
- Patients with adequate respiratory effort use CPAP for positive pressure ventilation
- If wheezing present see Acute Broncospasm protocol
- Consider CPAP to achieve FiO2 of 100% to expedite clearance
- IV 0.9% NaCl KVO or IV lock
- If BP < 90 mm Hg systolic, administer boluses of 0.9% NaCl at 250 ml until systolic BP > 90 mm Hg
- Contraindicated if evidence of congestive heart failure (e.g. rales)
- If no response, administer Push dose epinephrine: Remove 9ml (0.9mg) of 1:10,000 Epinephrine from the pre-filled syringe then draw 9ml of NS into the pre-filled syringe and mix solution. Concentration 10mcg/ml. IV push 1ml every minute to increase blood pressure to 90 mmHg; max 10ml (100mcg).
Transport Guidelines
- Patients with suspected or known exposure to CO presenting with clinical signs and symptoms MUST BE TRANSPORTED to the closest appropriate facility
- Patients evaluated for possible CO exposure who are competent to make decisions, have no medical complaints, and are not experiencing any signs or symptoms may refuse care and transportation if the following criteria are met and documented:
- Two sets of vital signs that are within normal limits (10 minutes apart)
- SpCO2 level of less than 20% on two readings (10 minutes apart)
- Document a refusal of care according to patient refusal protocol
Carbon monoxide Bloodstream Levels
- Reference Range
- Non-Smoker < 2%
- Smoker < 10%
Clonidine (Alpha-2 Adrenergic agonist) Overdose
Example of commonly used alpha-2 adrenergic agonists:
- Clonidine (Catapress)
- Imidazoline
Advanced Life Support
- Full ALS Assessment and Treatment
- Toxidrome includes central nervous system depression, bradycardia, hypotension, respiratory depression, and small pupil size. For severe central nervous system or respiratory depression:
- Naloxone (Narcan) 2 mg IV (start at 0.4 mg for patients over 65 years old)
- Naloxone (Narcan) can be given in 0.4 mg increments, titrated to mental status and respiratory drive (monitor respiratory status with continuous capnography)
- If respiratory depression persists, repeat every 3 minutes to a maximum of 8 mg
- If IV access has not been established, Naloxone (Narcan) can be given IM/IO or via mucosal atomizer device
- If hypotensive, administer 250ml fluid boluses until BP > 90 mm Hg.
- If still hypotensive, administer Push dose epinephrine: Remove 9ml (0.9mg) of 1:10,000 Epinephrine from the pre-filled syringe then draw 9ml of NS into the pre-filled syringe and mix solution. Concentration 10mcg/ml. IV push 1ml every minute to increase blood pressure to 90 mmHg; max 10ml (100mcg).
- Naloxone (Narcan) 2 mg IV (start at 0.4 mg for patients over 65 years old)
Cocaine and Sympathomimetic Overdose
Advanced Life Support
- Full ALS Assessment and Treatment
- For patients with sympathomimetic toxidrome (hypertension, tachycardia, agitation):
- Midazolam (Versed) 5 mg IM or intranasal via MAD OR 2.5 mg IV
- Repeat Midazolam (Versed) 5 mg IM or intranasal via MAD OR 2.5 mg IV if adequate sedation not achieved on initial dose
- Midazolam (Versed) 5 mg IM or intranasal via MAD OR 2.5 mg IV
- If seizures occur, refer to Seizure Protocol fix format
Cyanide Toxicity and Smoke Inhalation
Cyanide poisoning may result from inhalation, ingestion or dermal exposures to cyanide containing compounds, including smoke from closed-space fires. The presence and extent of the poisoning are often unknown initially. Treatment decisions must be made on the basis of clinical history and signs and symptoms of cyanide intoxication. Not all patients who have suffered smoke inhalation from a closed space fire will have cyanide poisoning. Other conditions such as burns, trauma or other toxic inhalations (e.g. carbon monoxide) may be the cause of symptoms. When smoke inhalation is the suspected source of cyanide exposure assess the patient for the following:
- Exposure to fire or smoke in an enclosed space
- Presence of soot around the mouth, nose or oropharynx
- Altered mental status
Common Signs and Symptoms of Cyanide Toxicity
- Headache
- Altered mental status
- Confusion
- Seizures
- Coma
- Dyspnea
- Respiratory distress/apnea
- Tachypnea
- Chest pain or tightness
- Nausea/vomiting
- Hypertension (early)
- Hypotension (late)
- Cardiovascular collapse/cardiac arrest
Advanced Life Support
- Supplemental 100% Oxygen
- Including ETCO2 level (35-45 normal)
- Perform Full ALS Assessment and Treatment
- When clinical suspicion of Cyanide poisoning is present:
- Hydroxocobalamin (Cyanokit) 5 grams or two 2.5 grams vials IV/IO over 15 minutes
- Use NaCl 0.9% as diluent for Cyanokit as per manufacturer instructions
- Contraindicated in patients with known anaphylactic reactions to hydroxocobalamin or cyanocobalamin
- If severe symptoms persist, contact Medical Control for consideration of additional dose of Cyanokit 5 gram IV/IO over 15 minutes (only if patient in extremis)
- Hydroxocobalamin (Cyanokit) 5 grams or two 2.5 grams vials IV/IO over 15 minutes
- Expedite transport and treat other conditions as per appropriate protocols
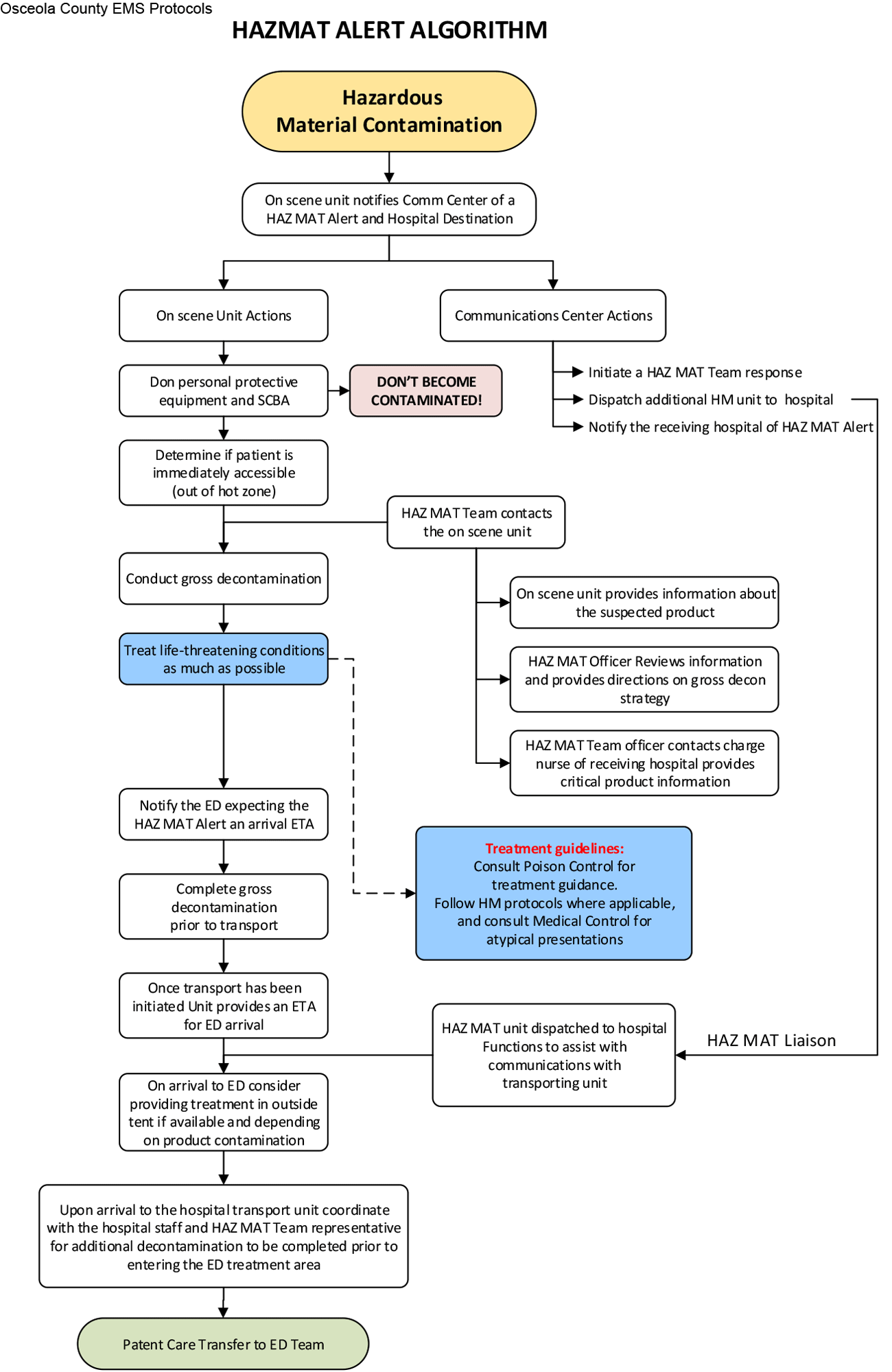
HAZMAT Alert
Guiding Principle
To create a standard method of patient care for incidents involving patients exposed to, or suspected to have been exposed to, a Hazardous Substance or Hazardous Material. By declaring a HAZMAT Alert a pre-planned series of events will take place to protect the patient, our personnel, and the receiving facility’s personnel. A HAZMAT Alert will provide the following:
- Early notification to receiving hospitals of an incoming HAZMAT patient.
- Early involvement of the closest HAZMAT Team in decision-making.
- Early involvement of Regional Poison Control or Medical Control.
Procedures
- A HAZMAT Alert should be initiated:
- At the time of dispatch, when a caller reports a medical emergency involving a chemical smell or hazardous material exposure.
- When the first arriving crew suspects a hazardous materials exposure due to odor, history, or other sources of information.
- By hospital Emergency Department staff in the event a hazardous material exposure is suspected from a walk-in patient and additional resources are needed.
- Actions after a Hazardous Materials Exposure has been recognized:
- Immediately contact the Communications Center and initiate a HAZMAT Alert.
- Advise the Communications Center of the transport destination as soon as possible.
- Ensure all personnel are wearing the appropriate PPE.
- After acknowledgement of a HAZMAT Alert, the Communications Center will:
- Notify the closest available HAZMAT Team to the incident.
- Provide a "heads-up" notification to the receiving facility.
- If requested by the Emergency Department the Communications Center can place the receiving facility on Condition Black until it is determined to be safe to resume normal EMS transports.
- Once notified of a HAZMAT Alert the agency HAZMAT Team will contact the on-scene crew to accomplish the following:
- Identify and research the hazardous material.
- Determine if HAZMAT Team response is needed.
- Advise on-scene crews of level of PPE required.
- Determine the nature of exposure and appropriate decontamination procedures.
- Advise on treatment in conjunction with Poison Control and local EMS protocols.
- Determine and advise when transport can be safely initiated for the patient and personnel.
- The HAZMAT Team Leader will make contact with the receiving facility and pass on all appropriate information about the patient, hazardous material involved, PPE and decontamination procedures as necessary.
- Determine if a liaison is required to respond to the receiving facility and recommend to the agency the appropriate liaison (i.e., Chief Officer, HAZMAT Team, etc.)
- Transfer of care:
- Prior to arrival at the Emergency Department transporting crews should contact the Emergency Department or Fire Department liaison to convey pertinent information on the patients exposure, condition and the specifics of the decontamination strategy employed on the scene.
- Before entering the Emergency Department, allow the hospital staff to assess the need for further decontamination.
Tricyclic and Tetracyclic Antidepressant Overdose
Advanced Life Support
- Full ALS Assessment and Treatment
- If wide QRS complex (≥0.10 sec), hypotension, or any arrhythmias:
- Sodium Bicarbonate 1 mEq/kg IV
- Repeat Sodium Bicarbonate 1 mEq/kg IV in 5 to 10 minutes
- For hypotension (systolic BP < 90 mmHg) not improved by fluid boluses, or when fluid boluses are contraindicated:
- Norepinephrine infusion at 0.5-16 mcg/minute IV/IO, titrated to maintain SBP > 90 mm Hg (see pg. 10-27 for infusion preparation chart) OR
- Push dose epinephrine: Remove 9ml (0.9mg) of 1:10,000 Epinephrine from the pre-filled syringe then draw 9ml of NS into the pre-filled syringe and mix solution. Concentration 10mcg/ml. IV push 1ml every minute to increase blood pressure to 90 mmHg; max 10ml (100mcg).
- If any of the following conditions occur, refer to the appropriate protocols:
- Polymorphous Ventricular Tachycardia
- Altered mental status
- Seizures
Contact Medical Control for Additional Orders if Needed

